- Overview
- Symptoms
- Causes & Risks
- Tests & Diagnosis
- Treatment
- Living With
- Complications
- Support & Resources
- Appointment Prep
- View Full Guide
Crohn's and Arthritis


Crohn's and Joint Pain
Arthritis is the most common complication outside the intestines for people with Crohn's disease. About 30% of people with Crohn's experience joint pain. When your gut is inflamed, it can trigger inflammation in your joints too. This connection is part of what doctors call "extraintestinal manifestations" -- symptoms outside your digestive tract.

Types of Arthritis Linked to Crohn's
Two main types of arthritis affect people with Crohn's disease: peripheral arthritis (affecting knees, ankles, wrists) and axial arthritis (affecting the spine). Peripheral arthritis often flares up with intestinal symptoms, while axial arthritis, including ankylosing spondylitis, typically follows its own course independent of gut inflammation.

Recognizing Peripheral Joint Symptoms
Peripheral arthritis in Crohn's typically causes pain, swelling, and stiffness in large joints like knees, ankles, elbows, and wrists. These symptoms often appear alongside digestive flares and may improve when your Crohn's is under control. Unlike rheumatoid arthritis, this type rarely causes permanent joint damage but can significantly impact your daily life.

Understanding Axial Arthritis Signs
Back pain that improves with exercise but worsens with rest is a hallmark of axial arthritis. You might notice stiffness in your lower back, especially in the morning or after inactivity. Unlike peripheral arthritis, these symptoms often develop independently of your Crohn's flares and may continue even when your digestive symptoms are under control.

Ankylosing Spondylitis and Crohn's
Ankylosing spondylitis is a serious form of spinal arthritis. Estimates vary, but it is believed to affect between 2% and 6% of people with Crohn's. It causes inflammation where ligaments and tendons attach to bones, particularly in your spine and pelvis. Over time, it can lead to fusion of spinal vertebrae. Early symptoms include ongoing lower back pain, especially at night and in the morning.
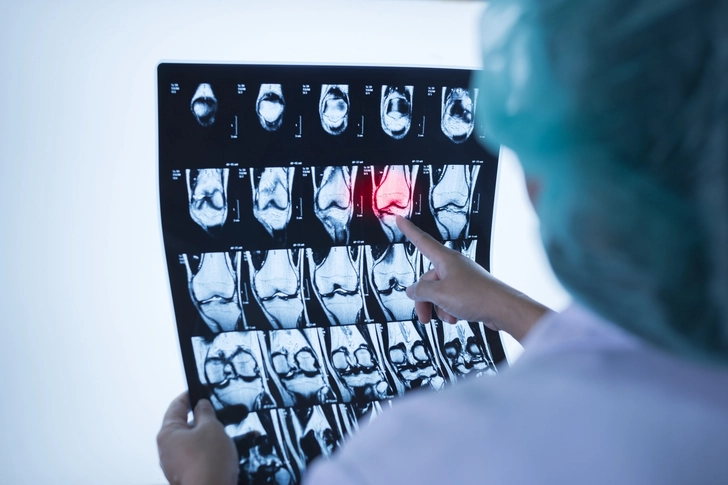
How Doctors Diagnose Joint Problems
If you have Crohn's and joint pain, your doctor may recommend blood tests to check for inflammation markers and imaging tests like X-rays or MRIs. They'll rule out other causes of joint pain and may refer you to a rheumatologist, a doctor who diagnoses and treats arthritis. You can help the doctor by describing when your pain occurs, which joints hurt, and how the pain relates to your digestive symptoms.

Treating Both Conditions Together
Some medications can help both Crohn's and arthritis symptoms. Biologics like TNF inhibitors target inflammation in both the gut and joints. Corticosteroids can provide short-term relief during flares, while immunomodulators help prevent flares. Your doctor will create a treatment plan addressing both conditions while minimizing side effects.

Self-Care Strategies for Joint Pain
Gentle exercise like swimming or walking can help your joints feel better without stressing your digestive system. Apply heat for stiffness and cold for acute pain. Maintain good posture and consider seeing a physical therapist to get specific exercises for your joints. You can rest during severe flares, but don't be inactive for too long, as this can make you stiffer. Stay at a healthy weight to reduce the stress on your joints.

When to Call Your Doctor
Let your health care provider know if you develop new joint pain, especially with swelling or limited movement. Seek immediate care for severe, sudden pain or inability to move a joint. Regular checkups help monitor both conditions. Let your doctor know about all your symptoms, even those that don't seem related to digestion, because that can help your doctor make treatment decisions.
PHOTO CREDENTIALS
Slide 1 - Sorapop Udomsri / Shutterstock
Slide 2 - DimaBerlin / Shutterstock
Slide 3 - Dragana Gordic / Shutterstock
Slide 4 - Perfect Wave / Shutterstock
Slide 5 - staras / Shutterstock
Slide 6 - Komsan Loonprom / Shutterstock
Slide 7 - Prostock-studio / Shutterstock
Slide 8 - Lordn / Getty Images
Slide 9 - DariaPotapova / Shutterstock
SOURCES
Gastroenterology and Hepatology: “Management of Arthritis in Patients with Inflammatory Bowel Disease.”
Crohn’s and Colitis Foundation: “Arthritis,” “Arthritis and Joint Pain,” “Small and Large Bowel Resection.”
Crohn’s and Colitis Canada: “Joint Inflammation and Arthritis.”
Stat Pearls: “Seronegative Spondyloarthropathy.”
Johns Hopkins Medicine: “Colectomy.”
Annals of the Rheumatic Diseases: "Incidence of Inflammatory Bowel Disease in Patients with Ankylosing Spondylitis."
Arthritis Research & Therapy: "A Longitudinal Study of Fecal Calprotectin and the Development of Inflammatory Bowel Disease in Ankylosing Spondylitis."
Best Practice & Research: Clinical Rheumatology: "Ankylosing Spondylitis and Bowel Disease."
Canadian Digestive Health Foundation: "What is the Fecal Calprotectin Test?"
Crohn's and Colitis Canada: "Ankylosing Spondylitis."
Frontiers in Genetics: "Bidirectional Causal Associations Between Inflammatory Bowel Disease and Ankylosing Spondylitis: A Two-Sample Mendelian Randomization Analysis."
GI Society: "Co-Managing IBD & Arthritis: A Complex Prescription," "Fecal Calprotectin Test."
Johns Hopkins Medicine: "Ankylosing Spondylitis."
Mayo Clinic: "Crohn's disease."
MedlinePlus: "HLA-B27 Antigen," "NOD2 Gene."
National Institute of Diabetes and Digestive and Kidney Diseases: "Treatment for Crohn's Disease."
PeerJ: "Association of Crohn's disease-related chromosome 1q32 with ankylosing spondylitis is independent of bowel symptoms and faecal calprotectin."
World Journal of Gastroenterology: "Inflammatory Bowel Diseases and Spondyloarthropathies: From Pathogenesis to Treatment."
Spondylitis Association of America: “Medications Used to Treat Ankylosing Spondylitis and Related Diseases.”