- Overview
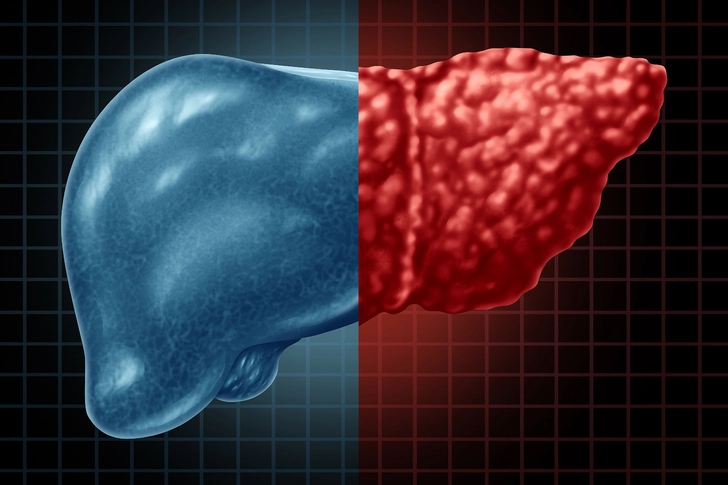
- MASLD and MASH
- Tests & Diagnosis
- Treatment and Prevention
- Complications
- Appointment Prep
- View Full Guide
Your MASH Diagnosis and What Your Test Results Really Mean



Making Sense of Your Lab Tests After Your MASH Diagnosis
With metabolic dysfunction-associated steatohepatitis (MASH), you're likely a pro at blood tests. You may know what some mean, but other tests may look like a jumble of letters and numbers. Review the tests that helped diagnose your MASH, like the complete blood count (CBC) and liver function test (LFT).
Find out how your doctor adds these numbers up to estimate your risk score for liver scarring, also called fibrosis. Learn to decode all those lab reports and discover how they monitor your condition to prevent cirrhosis, serious liver damage.

Liver Function Testing Can Help Prevent Liver Damage
The same liver function test that helped diagnose your MASH can monitor your disease progress, trigger treatment, and prevent serious liver damage. The test looks at levels of proteins, waste by-products, and certain enzymes to check how well your liver is working. Your doctor will add your LFT levels to other tests, imaging, and biopsy results to:
- Estimate liver fibrosis
- Monitor your MASH
- Decide when to start treatment
- Diagnose cirrhosis

Can Your Liver Function Test (LFT) Diagnose MASH?
Your LFT can't diagnose MASH alone, but the test can estimate your fibrosis risk as your disease progresses. Some key liver enzymes, substances, and proteins are:
- Alanine aminotransferase (ALT)
- Aspartate aminotransferase (AST)
- Gamma-glutamyl transferase (GGT)
- Bilirubin
- Albumin
During the later stages of MASH, your ALT can get up to15 times higher than normal (but not for everyone). Higher liver enzymes are a clue for your doctor to do more tests.

Will I Still Need a Complete Blood Count (CBC)?
A CBC helps your doctor calculate your fibrosis index based on four factors (FIB-4) score and check other health problems. This test measures your blood cells and more, but your doctor mainly looks at your platelet levels (cell-like bits that form blood clots). You may be at risk for liver scarring with lower than normal platelets – also called thrombocytopenia.
Is the FIB-4 Score Still Useful?
You already know that your doctor uses the Fib-4 score which often prevents unneeded biopsy. But the score also monitors your disease progression. FIB-4 scores can guide your doctor in the next best steps and estimate liver fibrosis risk:
- Low. Below 1.3
- Medium. Between 1.3 and 2.67
- High. Above 2.67
Your doctor will probably repeat a low score in 2-3 years. A medium risk can prompt liver stiffness testing, but a high score can mean seeing a liver specialist.

Can an Ultrasound Show Liver Scarring?
Your doctor may have ordered an ultrasound with high-intensity sound waves when you were diagnosed. The image may have showed:
- Extra fat buildup in your liver that was brighter than normal
- Serious liver damage that showed up as lumps or a shrunken liver
You may get a mild, moderate (medium), or serious steatosis (fat) score – a liver fat estimate. But your doctor also checks your FIB-4 score and may order a special type of ultrasound to make sure.

What Is Ultrasound Elastography?
As your condition progresses, ultrasound elastography can estimate your liver fibrosis and stiffness. Using transient and shear waves, the ultrasound bounces sound off your liver which vibrates. But scarred livers are harder, and don't move normally. One common brand, FibroScan, adds a blood test called the enhanced liver fibrosis (ELF) score to estimate your fibrosis risk:
- Medium, 8-12 kilopascals (kPa), ELF 7.7-9.8.
- High, above 12 kPa, ELF above 9.8.
Your doctor can also use a FibroScan plus CAP (percent change in fat):
- Medium, 7.5-10 kPa, fibrosis score F2.
- Serious, 10-14 kPa, F3.

Other Ways to Check Liver Stiffness and Fibrosis
If you have later stage liver disease, your doctor may refer you to a gastroenterologist – a liver and stomach specialist. The specialist may order more tests, such as:
- Liver biopsy to measure liver inflammation, scars, and fat.
- AST-to-platelet ratio index (APRI) where scores above 1.5 mean a higher fibrosis risk.
- FibroSure or FIBROSpect II, which can take into account age, gender, or various proteins like GGT, bilirubin, and ALT.
- Nonalcoholic fatty liver fibrosis score (NFS) to estimate liver scarring.

With a Higher Risk of Fibrosis, Will I Need a Liver Biopsy?
If some of your liver scores don't add up or your doctor needs a closer look at your liver, you may get a liver biopsy. Your doctor uses a needle to remove a small bit of liver tissue for testing. Under a microscope, they'll check for inflammation, fat buildup, and fibrosis. There are different scoring systems, but your biopsy report may mean:
- F1, mild stiffness
- F2, medium fibrosis
- F3, serious fibrosis
- F4, serious scarring (cirrhosis)
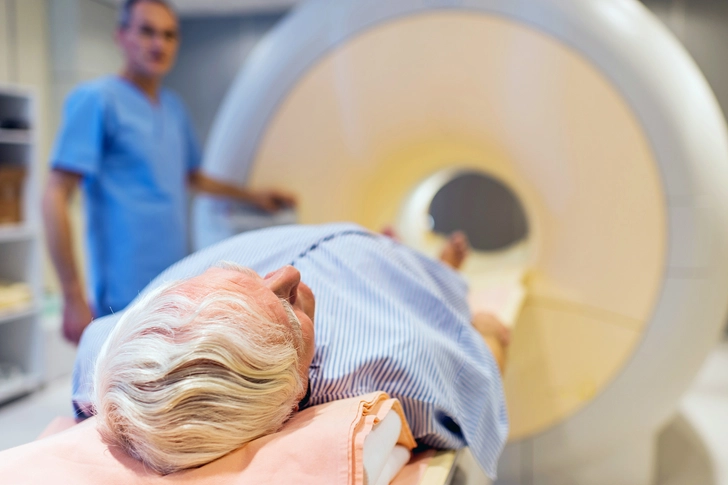
Why Do I Need an MRI for My Liver?
If your doctor suspects your condition has progressed to a later stage, you may get an MRI. There are a few types of MRI that can estimate your MASH and fibrosis risk:
- Magnetic resonance elastography (MRE) uses MRI and sound waves (elastography) to move your liver because stiffer, scarred parts don't move normally.
- MRI-PDFF. Proton density fat fraction (PDFF) measures the percentage of fat in your liver.
- Corrected T1 MRI (cT1 MRI) measures liver inflammation along with fibrosis, but newer methods can tell the two apart.

Will I Need Other Blood Tests to Monitor MASH?
Yes, other CBC and LFT markers can help estimate and monitor scarring:
- High GGT
- Low albumin
- Longer clotting time – prothrombin time (PT) or international normalized ratio (INR)
MASH is also linked to type 2 diabetes, diseases of the heart and blood vessels, and kidney disease. Your doctor may check your:
- HbA1c
- Glucose
- HDL (good) cholesterol
- Triglycerides
- Estimated glomerular filtration rate (eGFR)
- Creatinine
- Blood urea nitrogen

What Can Iron Studies Tell You?
Iron studies can tell you if your MASH has progressed enough to possibly cause insulin resistance. That's because your liver stores iron which controls insulin receptors (protein structures that help insulin act on your cells). Liver fibrosis can trigger higher iron levels that block your insulin receptors and cause insulin resistance. With MASH, your total iron-binding capacity (TIBC) studies may show:
- Iron levels above 145 micrograms per deciliter (mcg/dL) for women and above 150 mcg/dL for men
- Ferritin levels above 205 nanograms per milliliter (ng/mL) for women or above 566 ng/mL for men
- Transferrin saturation (percentage of iron bound to the protein transferrin) above 45%

What Other Tests Monitor Liver Health?
Your doctor can add certain tests together to better estimate your risk for inflammation, fibrosis, and liver damage. In fact, they may have estimated your risk for MASH using one of these combined scores. Your risk for MASH was very likely if you had a:
- FibroScan and AST (FAST) score above 0.67
- MRI with AST (MAST) score above 0.242
- FIB-4 score above 1.6 and MRE above 3.3 kPa on an MRE with FIB-4 (MEFIB)
- cT1 MRI score above 875 milliseconds (ms), but you'll need more testing

Which Tests Can Detect Advanced Liver Fibrosis?
Your doctor uses some blood tests and imaging scans to estimate your risk of moderate to serious liver scarring. You may have a higher risk of advanced liver scarring if your:
- FIB-4 score is above 2.67
- NSF score is above 0.672
- ELF score is above 9.8
- FIBROSpect II score is above 17
- FibroScan score is F3 or F4
- MRE score is above 3.63 kPa

How Does My Doctor Test for Cirrhosis Risk?
If your condition worsens, your doctor uses the scores to monitor your treatment progress and keep an eye on any higher cirrhosis risk scores, such as:
- FIB-4 above 3.48
- ELF above 11.3
- MRE above 5 kPa
- FibroScan-CAP above 14 kPa and F4, or VCTE above 20 kPa
With higher risk for cirrhosis, you'll talk with your doctor about the next step. If you have any questions about testing, ask your doctor to explain or see if a change in treatment can help.
IMAGES PROVIDED BY:
1) iStock/Getty Images
2) iStock/Getty Images
3) iStock/Getty Images
4) iStock/Getty Images
5) iStock/Getty Images
6) iStock/Getty Images
7) Ahmad Amin M/Radiopaedia.org
8) Gumpanat/Shutterstock
9) E+/Getty Images
10) E+/Getty Images
11) iStock/Getty Images
12) iStock/Getty Images
13) iStock/Getty Images
14) iStock/Getty Images
15) DigitalVision/Getty Images
SOURCES:
UpToDate: "Pathogenesis of metabolic dysfunction-associated steatotic liver disease (nonalcoholic fatty liver disease), " "Approach to the patient with abnormal liver tests."
Mayo Clinic: "Liver Function Tests."
American Liver Foundation: "MASH Diagnosis."
Cleveland Clinic: "Complete Blood Count (CBC)," "Ultrasound."
Liver International: "Platelet Functional Profile Is Altered in Metabolic Dysfunction‐Associated Steatotic Liver Disease."
Free Radical Biology and Medicine: "Iron overload exacerbates metabolic dysfunction-associated steatohepatitis via the microbiota-gut-liver axis through lipopolysaccharide-mediated Akr1b8 activation."
American Association of Clinical Endocrinology (AACE): "AACE Patient Guide to Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) and Metabolic Dysfunction-Associated Steatohepatitis (MASH)."
National Lipid Association: "Practical Pearls: Dyslipidemia Management in Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD)."
RadiologyInfo.org: "Fatty Liver Disease and Liver Fibrosis."
LapCorp: "NASH/NAFLD: Screening and Diagnostic Testing."
Associates in Gastroenterology Endoscopy Centers of Colorado Springs: "What is FibroScan?"
Journal of Clinical and Experimental Hepatology: "Non-alcoholic Fatty Liver Disease and Metabolic Syndrome – Position Paper of the Indian National Association for the Study of the Liver, Endocrine Society of India, Indian College of Cardiology and Indian Society of Gastroenterology."
JHEP Reports: "Enhanced liver Fibrosis test predicts liver-related outcomes in the general population."
BMC Gastroenterology: "Evaluation of NAFLD and fibrosis in obese patients – a comparison of histological and clinical scoring systems."
Journal of Infectious Diseases: "Elevation of Liver Fibrosis Index FIB-4 Is Associated With Poor Clinical Outcomes in Patients With COVID-19."
The Journal of the American Medical Association: "Performance of the Enhanced Liver Fibrosis Test to Estimate Advanced Fibrosis Among Patients With Nonalcoholic Fatty Liver Disease."
Nature Communications: "Practical diagnosis of cirrhosis in non-alcoholic fatty liver disease using currently available non-invasive fibrosis tests."
American Family Physician: "Nonalcoholic Fatty Liver Disease: Diagnosis and Management," "Nonalcoholic Fatty Liver Disease: Diagnosis and Management Guidelines From the AACE."
World Journal of Hepatology: "Liver function tests and metabolic-associated fatty liver disease: Changes in upper normal limits, does it really matter?"
Molecular Metabolism: "Imaging biomarkers of NAFLD, NASH, and fibrosis."
Gastrointestinal Imaging: "Beyond the Liver Function Tests: A Radiologist's Guide to the Liver Blood Tests."
Hepatology: "Guideline-based management of metabolic dysfunction-associated steatotic liver disease in the primary care setting," "AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease."
Memorial Sloan Kettering: "Understanding Your Liver Elastography (FibroScan) Results."
Diagnostics: "Diagnostic Modalities of Non-Alcoholic Fatty Liver Disease: From Biochemical Biomarkers to Multi-Omics Non-Invasive Approaches."
International Journal of Molecular Science: "NAFLD (MASLD)/NASH (MASH): Does It Bother to Label at All? A Comprehensive Narrative Review."